
A lot of things can happen to put you in the market for a new doctor. Maybe you’ve moved to a new town and need to find a pediatrician for your kids’ well-visits. Or your primary care physician (PCP) recommends you follow-up with a specialist. Or you’ve turned 45 and are due to get your first colonoscopy. Whatever the reason, you want to be sure you’re choosing the right doctor.
All health insurance plans have a network of doctors, and selecting one who is in that network can save you money. In fact, some plan types require you to see an in-network provider. So, how do you find a provider who’s in your health plan’s network?
Recommendations from friends, family, and your PCP are a great place to start. Your next stop should be our Find a Doctor tool, which makes it easy to find in-network doctors and other health care providers, such as labs, hospitals, urgent care centers, and outpatient surgery centers. Review the questions and answers below to help you understand the difference between in-network and out-of-network and how to choose a doctor.
What is a provider?
A health care provider is a person or company that delivers a health care service to you. Types of providers include your primary care physician (PCP), specialists, and even facilities, like labs, hospitals, and urgent care centers. POLICY BRIEF ON OUT-OF-NETWORK BILLING
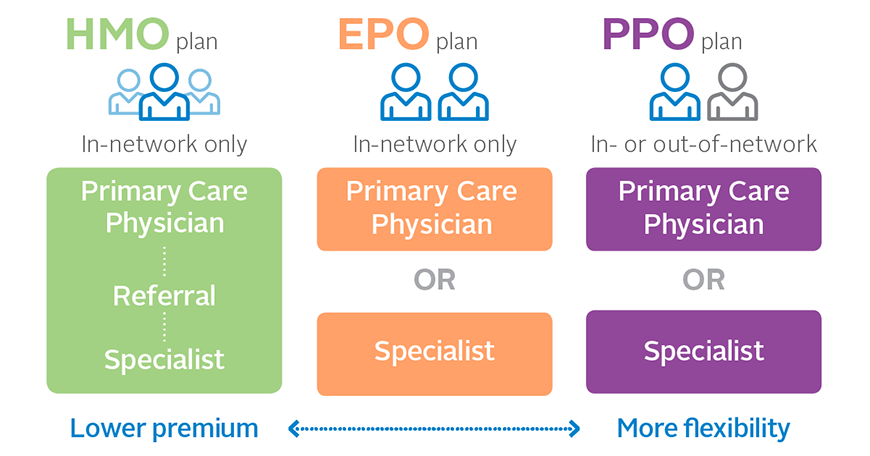
What does in-network mean?
In-network refers to a health care provider that has a contract with your health plan to provide health care services to its plan members at a pre-negotiated rate. Because of this relationship, you pay a lower cost-sharing when you receive services from an in-network doctor. In-Network vs. Out-of-Network Providers | Cigna Healthcare
What does out-of-network mean?
Out-of-network refers to a health care provider who does not have a contract with your health insurance plan. If you use an out-of-network provider, health care services could cost more since the provider doesn’t have a pre-negotiated rate with your health plan. Or, depending on your health plan, the health care services may not be covered at all. Not in the health plan's network of selected and approved doctors and hospitals. Members who get care out-of-network (sometimes called out-of-area) without ...
How do I know if a doctor is covered by my insurance?
Use the Find a Doctor tool and start searching! Enter your location and health plan, and your search will return results that only include providers who are in your network.
Is it more expensive to see a provider outside of my health plan’s network?
Yes, typically you’ll pay more if you go to an out-of-network provider. Keep in mind that some health plans don’t have any coverage for non-emergency services received from an out-of-network provider. Be sure to check your benefits before picking a doctor or other health care provider.
What are the benefits of choosing providers in the Independence Blue Cross network?
With the Independence Blue Cross network, you have access to the largest network of doctors and hospitals in the region, with more than 60,000 doctors and 180 hospitals. In addition to paying lower out-of-pocket-costs, you also have the security of knowing we have screened the providers in our network to ensure they meet our quality standards.

 You may be eligible to apply for an affordable health plan today.
You may be eligible to apply for an affordable health plan today.
 Get Medicare plans from Independence.
Get Medicare plans from Independence.






